Help Us Get Our Lives Back
/By Andrea Giles, Guest Columnist
I am a 49-year old disabled nurse living in Wyoming. Since 2010, I have been diagnosed with ankylosing spondylitis, phantom limb pain and severe osteoarthritis with multiple major joint deformities. My remaining knee is now bone on bone, requiring me to use a wheelchair.
I lost my right leg and half of my pelvis after a total hip replacement due to the osteoarthritis, after which I developed a severe MRSA bacterial infection that resulted in the total hip disarticulation. I’ve had horrible phantom limb pain since the amputation. I also had 2 failed spinal fusions, leaving me with chronic back pain and nerve damage. Since 2010, I have had a total of 52 surgeries.
From 2010 to 2016, I was treated with opioid medication by a pain management physician, with a stable, safe, effective and legal regimen. I followed all of the requirements, such as urine drug tests, pill counts, using the same pharmacy, etc.
Then, at an appointment in 2016, my physician told me that because of the CDC guidelines, he would no longer prescribe opioid medication to me. I was forced off my high dose (120MME) cold turkey. I was lucky, as I didn’t experience withdrawal symptoms other than the reappearance of severe, intractable pain.
I tried to use NSAIDS for the pain and developed a severe, life threatening reaction to them called Stevens-Johnson Syndrome. I came very close to death and was in intensive care for 6 weeks. Because of that, I will be unable to take NSAIDs for the rest of my life.
Because of the MRSA infection, no physician will perform any further surgeries or steroid injections on me because of the risk of activating another infection.
I have tried acupuncture, massage, chiropractic therapy, mirror therapy, physical therapy, water therapy, many different herbal and nutritional supplements, aromatherapy, music therapy, psychotherapy, hypnotherapy and mindfulness. All without relief of the severe, intractable pain.
When I was forced off opioids, I also lost my career as a very good ER nurse. I went from a functional member of society to a home-bound, miserable person who hurts too badly to keep my house clean like I always prided myself on. Many days I’m in too much pain to even shower or complete daily activities of living.
My husband and children have lost the wife and mother they were able to interact with, go places with, share activities with, everything. I have gained 50 pounds because the pain has left me unable to exercise.
After I stopped taking opioids, I developed hypertension. Before, my blood pressure had never been higher than 130/80. Now I take medication for high blood pressure and it is still usually around 150/90.
I also developed heart arrhythmia and last year suffered 2 sudden cardiac arrests. I only survived because both times they were witnessed by my husband, who is also an ER nurse, so he immediately started CPR. The cardiologist could find no underlying causes and told me that the arrhythmia and cardiac arrests were probably due to longstanding, untreated severe pain.
There is no physician that I can find that will accept me as a chronic pain patient and my primary care doctor refuses to prescribe opioids anymore. I have literally tried every pain management physician in Wyoming and in Montana, which would have required a 6 to 7-hour drive for each appointment.
I, along with many other intractable pain patients, are working feverishly contacting our congressional representatives, federal government and civil rights groups, begging for help -- for anyone in a position of power to hear our cries of medical abandonment and neglect.
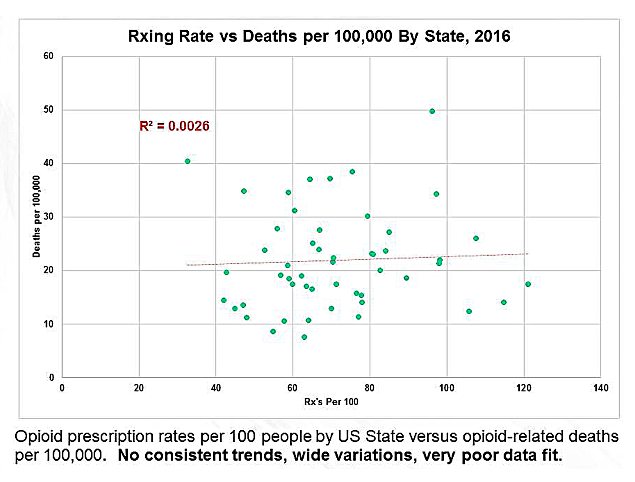
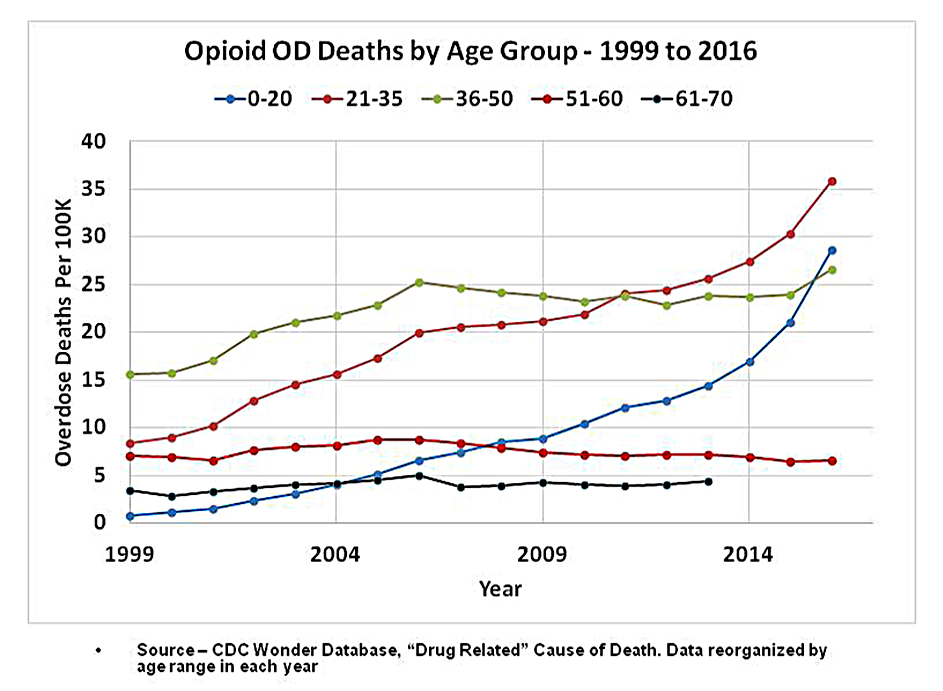
Our pleas mostly fall on deaf ears, as the government has convinced the media and the public that pain patients are all addicts and use opioids only to get high. They site false overdose statistics and refuse to acknowledge that while opioid prescriptions have declined -- causing devastating effects on the pain community -- the overdose rate continues to climb because the clear majority of overdoses are due to heroin, illicit fentanyl or polypharmacy with multiple drugs.
Many intractable pain patients are committing suicide because untreated pain takes away their quality of life and the will to live – something they had with legally prescribed and effective doses of opioid medication.
We are desperate. We don’t want to get high. We just want to make informed decisions with our physicians about our own healthcare, to regain access to opioid medication, and to get our lives back!
Andrea Giles lives in Wyoming with her family.
Pain News Network invites other readers to share their stories with us. Send them to editor@painnewsnetwork.org.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.