FDA Head Calls for ‘Aggressive Regulatory Action’ on Opioids
/By Pat Anson, PNN Editor
In the wake of a highly critical report on 60 Minutes, the head of the Food and Drug Administration has pledged that drug companies will be required to prove that opioid medications are effective long-term in treating chronic pain and do not cause addiction.
“We are going to impose a mandate on existing products… to answer the question that people have been posing for years: whether you have declining efficacy, and whether that declining efficacy can lead to addiction,” FDA Commissioner Scott Gottlieb, MD, told The Washington Post.
60 Minutes reported on Sunday that the FDA caved into lobbying by the pharmaceutical industry in 2001 by changing the warning labels on OxyContin and other opioid medications to indicate they were effective for “daily, around-the-clock, long-term (use).” Critics say there is no good evidence to support that claim.
“You're using high-dose, long-duration opioids when they've never been designed to do that. There's no evidence that they're effective. There's extreme evidence of harms and deaths when you use them,” said Ed Thompson, the president and founder of drug maker PMRS.
What 60 Minutes and most media outlets fail to report is that there are no good long-term placebo-controlled studies for any pain relievers, including non-opioid medications like Lyrica and Cymbalta or over-the-counter drugs like acetaminophen.
Most clinical studies for pain relievers are limited to a few weeks duration because longer studies that use placebos to treat severe pain are considered unethical.
Gottlieb declined a request from 60 Minutes for an interview, but told The Washington Post on Monday that the FDA would require drug makers to conduct new research on “all immediate, long-acting and extended-release opioid tablets taken by patients outside of health-care settings.” Studies would not be required for intravenous opioids used in hospitals to treat acute pain.
“It’s regrettable we didn’t do this many years ago,” Gottlieb said.
On Tuesday, Gottlieb doubled down on the agency’s mea culpa in a lengthy, 4,094 word essay that pledged the FDA would “learn from past mistakes” and take “a much more aggressive approach to regulatory action” involving opioids.
“In this epidemic, waiting for the accumulation of definitive evidence of harm left us a step behind a crisis that was evolving quickly,” Gottlieb said. “We don’t want to look back five years from now, at an even larger crisis, with regret that there were more aggressive steps that we could have taken sooner.
“To reduce the rate of new addiction we need to reduce exposure to opioids. This means rationalizing prescribing, which in turn means that not only must we take steps to make sure fewer prescriptions for opioids are written, but also that when these drugs are prescribed, it’s for a dose and duration of use that comports closely with the clinical circumstance and the medical need of the patient.”
The FDA is already working with the National Academies of Science, Engineering, and Medicine to develop new opioid prescribing guidelines by the end of the year for medical conditions such as tooth extractions and outpatient surgeries.
The new recommendations would not replace the controversial 2016 CDC guideline, but would supplement it. The CDC guideline takes a one-size-fits-all approach to chronic pain -- pain that lasts longer than three months -- and doesn't distinguish between pain from fibromyalgia, arthritis, neuropathy or other medical conditions.
Gottlieb said the FDA would also take steps in the first half of 2019 to introduce “blister packs” of opioids with a limited supply of one or two days for treating short-term, acute pain.
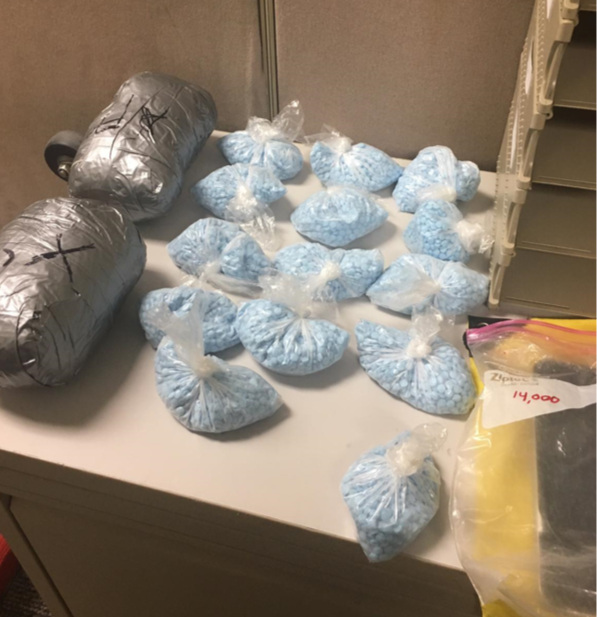
Opioid prescriptions have declined substantially since 2012, yet overdoses continue to soar, fueled in large part by illicit fentanyl, heroin and counterfeit medications. The Trump Administration is seeking to reduce opioid prescriptions by another third over the next three years.
If you haven’t already, this would be a good time to participate in PNN’s survey on the CDC guideline. We’re asking pain patients, as well as doctors and other healthcare providers, how the guideline has affected them and whether it should be revised. To take the survey, click here.