‘Radical Shift’ Predicted in Fibromyalgia Diagnosis and Treatment
/By Pat Anson, PNN Editor
New research has uncovered a previously unknown connection between fibromyalgia and the early stages of diabetes, which could dramatically change the way the chronic pain condition is diagnosed and treated.
In a small study of 23 fibromyalgia patients and two control groups, researchers at The University of Texas Medical Branch at Galveston (UTMB) were able to separate patients with fibromyalgia (FM) from healthy individuals using a common blood test for insulin resistance, or pre-diabetes. They then treated the fibromyalgia patients with a medication targeting insulin resistance (IR), which dramatically reduced their pain levels.
“Although preliminary, these findings suggest a pathogenetic relationship between FM and IR, which may lead to a radical paradigm shift in the management of this disorder,” researchers reported in the online journal PlosOne.
Fibromyalgia is a poorly understood disorder that causes widespread body pain, fatigue, insomnia, headaches and mood swings. The cause is unknown, the symptoms are difficult to treat and there is no universally accepted way to diagnose it.
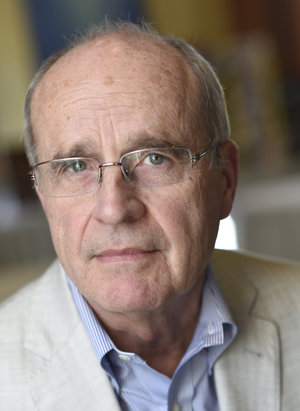
"Earlier studies discovered that insulin resistance causes dysfunction within the brain's small blood vessels. Since this issue is also present in fibromyalgia, we investigated whether insulin resistance is the missing link in this disorder," said Miguel Pappolla, MD, a professor of neurology at UTMB.
Pappolla and his colleagues found that patients with fibromyalgia can be identified by their hemoglobin A1c levels, a protein in red blood cells that reflects blood sugar levels. A1c tests are widely used to diagnose type 2 diabetes and pre-diabetes, and are routinely used in diabetes management.
Researchers say pre-diabetics with slightly elevated A1c levels carry a higher risk of developing widespread body pain, a hallmark of fibromyalgia and other chronic pain conditions.
"Considering the extensive research on fibromyalgia, we were puzzled that prior studies had overlooked this simple connection," said Pappolla. "The main reason for this oversight is that about half of fibromyalgia patients have A1c values currently considered within the normal range.
“However, this is the first study to analyze these levels normalized for the person's age, as optimal A1c levels do vary throughout life. Adjustment for the patients' age was critical in highlighting the differences between patients and control subjects."
After identifying the fibromyalgia patients with elevated A1c levels, researchers treated them with metformin, an oral medication that manages insulin resistance by restoring normal blood sugar levels. The patients showed dramatic reductions in their pain levels, with half (8 of 16 patients) having a complete resolution of pain.
“Our data provides preliminary evidence suggesting that IR may be a pathological substratum in FM and sets the stage for future studies to confirm these initial observations. If confirmed, our findings may translate not only into a radical paradigm shift for the management of FM but may also save billions of dollars to healthcare systems around the world,” researchers reported.